Author: Fernando Tejeda-Castro DO, PGY-1
Abstract
3,4-Methylenedioxymethamphetamine (MDMA), commonly known as “ecstasy” or “Molly”, has been used recreationally in the United States as a substitute for its analogue methylenedioxy-amphetamine (MDA).1 MDMA is an entactogen (meaning “producing a touching within”) that produces effects of enhanced pleasure, heightened sexuality, and expanded consciousness without the loss of control.2 A 25-year-old Spanish-speaking female presented to the emergency department (ED) after ingesting 10-15 “multicolored” pills which she believed to be ecstasy. Her urine drug screen was positive for cannabinoids and amphetamines. She was admitted to the general medical floor (GMF) where she had an isolated episode of severe tachycardia and agitation. She was evaluated by psychiatry after no persistent signs of sympathomimetic toxidrome or hyponatremia were noted.
Background
MDMA is called a “club drug” due to its frequent use by young adults at “raves” and dance parties due to its low dependence potential.1 MDMA differs from amphetamine and methamphetamine due to the presence of its methylenedioxy (-O-CH2-O-) group attached to positions 3 and 4 of the amphetamine aromatic ring, resembling the structure of the hallucinogen, mescaline.3 As a result, the pharmacological effects of MDMA resemble a blend of amphetamines and mescaline.3 MDMA’s sensory effects facilitate sociability, empathy, and a feeling of “togetherness,” whereas its energizing effects enable vigorous, long-term dancing.1 MDMA is typically taken orally in the form of capsules or tablets, or it can be snorted intranasally or injected.4 The typical recreational dose is approximately 3 mg/kg, and novice users usually take one or two tablets per occasion.4 The mechanism of action through which MDMA exerts is neurochemical effects includes MDMA binding to the serotonin, dopamine, and norepinephrine transporters thereby blocking the reuptake and promoting the release of each respective biogenic amine.4 Prominent symptoms of MDMA intoxication resulting from sympathetic stimulation include agitation, mydriasis, diaphoresis, hyperthermia, hypertension, and tachycardia.5 Hyperthermia is the most life-threatening manifestation and may be responsible for fatal sequelae including rhabdomyolysis, renal failure, and disseminated intravascular coagulation (DIC).5 Management of toxicity focuses on immediate treatment of hyperthermia and hypertension. For hyperthermia, passive, and environmental cooling to a temperature of 38.8 degrees Celsius is required.6 Further treatment is focused on correction of acidosis and electrolyte imbalance. MDMA is still used in the community and physicians should consider MDMA intoxication when patients present with signs of increased sympathetic and serotonergic activity. We present a case in which a 25-year-old Spanish-speaking female presented to the emergency department (ED) after ingesting 10-15 pills of ecstasy and was subsequently admitted for further monitoring.

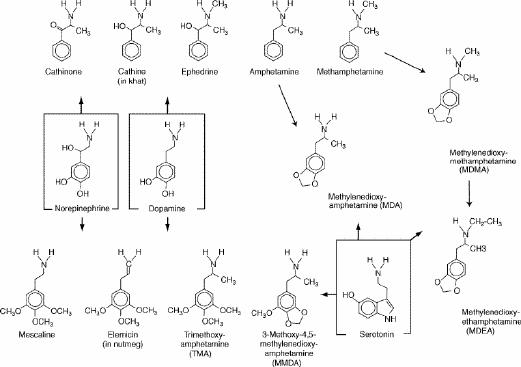
Figure 1: MDMA pills and the chemical structure of MDMA and related drugs. The arrows indicate the closest resemblances of structure.3
Case Description
A 25-year-old female presented to the ED after overdosing on ecstasy. In the ED, she was tachycardic with a rate of 132, and her temperature was 37.2 degrees Celsius . On physical examination, she appeared somewhat disheveled but was alert and oriented. Her pupils were dilated 5-6 millimeters bilaterally. No notable clonus, asterixis, rigidity of extremities, or diaphoresis was evident. An electrocardiogram was performed which showed sinus tachycardia with a rate of 132 beats per minute (Figure 1). Her laboratory analyses were unremarkable, and urine drug screen was positive for methamphetamine and cannabinoids. Treatment interventions in the ED included 1,000 mL of isotonic crystalloid fluids and 2 mg of IV lorazepam for agitation. The toxicology service was consulted, and the patient was admitted to the general medical floor (GMF). While in GMF around 2 AM, the patient became tachycardic to a heart rate of 200 and severely agitated. She was given 5 mg IM haloperidol and required 2 doses of 5 mg IV diazepam at 2 AM and 7 AM. At around 8 AM, the patient seemed to have returned to her baseline mental status but remained mildly somnolent. She admitted to taking pills to harm herself. No persistent signs of sympathomimetic toxidrome or hyponatremia were noted, and her heart rate was now 90-100. The patient was then evaluated by psychiatry. At the time of psychiatric evaluation, she no longer endorsed suicidal ideations and was thus cleared from a psychiatric standpoint. The patient was adamant about leaving the hospital at this time. However, her creatinine kinase was 9244 IU/L, and she was somnolent earlier that day. The psychiatry team was unable to convince the patient to stay for further observation. She proceeded to leave against medical advice.
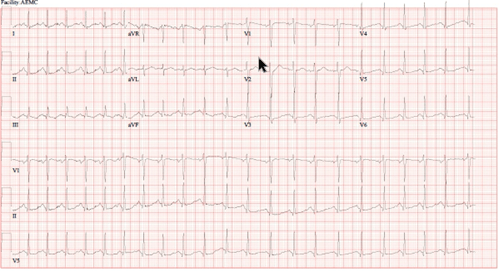
Figure 2: EKG showing sinus tachycardia with a rate of 132 but no evidence of acute ischemic changes or QT prolongation
Discussion:
This case highlights the importance of being aware of the clinical manifestations of acute MDMA toxicity and monitoring for sympathomimetic and serotonergic hyperstimulation. Close observation of temperature and adequate cooling measurements are paramount, given that it is the primary mechanism of fatality. A final point is the importance of monitoring electrolytes to assess for hyponatremia. There are two proposed mechanisms by which this occurs. First, dilutional hyponatremia is thought to occur in the setting of increased water intake and insensible losses due to environmental factures and thermodysregulation, exacerbating hyperthermia.6 The major mechanism for MDMA-induced hyponatremia has been attributed to an acquired syndrome of inappropriate antidiuretic hormone (ADH) secretion.6 MDMA can also increase the expression of aquaporin-2 channels in the inner medullary collecting duct of the kidney, which is involved in carrying water molecules across cell membranes. This then results in increased reabsorption of water independent of ADH levels.7
Learning Point #1: Clinical Manifestation
Acute administration of MDMA in doses ranging from 1 to 2 mg/kg leads to a constellation of physiological effects such as increased heart rate, blood pressure, and body temperature. MDMA has a plasma half-life of 8 to 9 hours, and after oral ingestion, desired effects typically between 1 hour and last between 4 and 6 hours.6 The acute effects of MDMA in users is primarily attributed to increased release and inhibited re-uptake of serotonin and norepinephrine, as well as possible release of neuropeptide oxytocin.4 Physically-desired effects include an increase in wakefulness, endurance, and energy.3 Psychological effects include greater sociability, closeness to others, and euphoria.6
Learning Point #2: MDMA and Serotonin Syndrome
MDMA increases serotonin release and inhibits serotonin reuptake at the synapses, resulting in a net increase in serotonin levels.6 Serotonin toxicity starts within a few hours and is characterized by a triad of clinical features including neuromuscular excitation, autonomic nervous system activation, and altered mental state.6 Increased muscle tone and rigidity, myoclonus, and increased deep tendon reflexes may be observed, along with gastrointestinal distress with vomiting and diarrhea due to stimulation of serotonin receptors in the gut.
Learning Point #3: MDMA and Adverse Effect of Hyperthermia
Most reported cases of hyperthermia and sequelae of rhabdomyolysis and multi-organ failure are associated with failed thermoregulation due to inadequate fluid replacement.6 As a result of inadequate fluid replacement, rhabdomyolysis, acute renal failure, DIC, and multiorgan failure can occur, often necessitating intensive care unit admission.8 Furthermore, no apparent dose-response relationship is seen with MDMA toxicity and hyperpyrexia, with cases reporting serum MDMA levels as high as 7.62 mg/L with no symptomatology and fatalities with levels as low as 0.11 mg/L.8 It’s important to consider that serum MDMA levels can appear lower if they are drawn following significant time since ingestion or if MDMA has already metabolized, which won’t necessarily correlate with symptomatology or toxicity. MDMA-related hyperthermia has been proposed to be serotonin-mediated, producing serotonin toxicity due to serotonin agonism and blockage of serotonin reuptake.
Learning Point #4: Management of MDMA Toxicity
Aggressive cooling measures with a goal temperature of at least 38.8 degrees Celsius and adequate resuscitation in patients presenting with hyperthermia is essential, and is considered the mainstay of treatment.6 Some systematic reviews have found evidence of decreased morbidity and mortality with the use of dantrolene in patients presenting with temperatures above 40 degrees Celsius, however this is widely debated.8 Seizures should be treated with benzodiazepines, and in unresponsive patients, definitive airway management via intubation and use of sedation is warranted.6 If a patient is hyponatremic, hypertonic saline should be considered.6
Citations
1. van Amsterdam , Jan, et al. “Fatal and Non-Fatal Health Incidents Related to Recreational Ecstasy Use.” Journal of Psychopharmacology (Oxford, England), U.S. National Library of Medicine, pubmed.ncbi.nlm.nih.gov/31909673/. Accessed 22 Oct. 2023.
2. Nelson, Lewis S., et al. “73.” Goldfrank’s Toxicologic Emergencies, McGraw-Hill Education, New York i Pozostałe, 2019.
3. Kalant, H. “The Pharmacology and Toxicology of ‘Ecstasy’ (MDMA) and Related Drugs.” CMAJ : Canadian Medical Association Journal = Journal de l’Association Medicale Canadienne, U.S. National Library of Medicine, 2 Oct. 2001, http://www.ncbi.nlm.nih.gov/pmc/articles/PMC81503/.
4. Meyer, Jerrold S. “3,4-Methylenedioxymethamphetamine (MDMA): Current Perspectives.” Substance Abuse and Rehabilitation, U.S. National Library of Medicine, 21 Nov. 2013, http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3931692/.
5. D;, Walubo A;Seger. “Fatal Multi-Organ Failure after Suicidal Overdose with MDMA, ‘Ecstasy’: Case Report and Review of the Literature.” Human & Experimental Toxicology, U.S. National Library of Medicine, pubmed.ncbi.nlm.nih.gov/10100025/. Accessed 22 Oct. 2023.
6. Davies, Nicola. MDMA Toxicity: Management of Acute and Life-Threatening Presentations, pubmed.ncbi.nlm.nih.gov/29894255/. Accessed 23 Oct. 2023.
7. Baggott, M. J., Garrison, K. J., Coyle, J. R., Galloway, G. P., Barnes, A. J., Huestis, M. A., & Mendelson, J. E. (2016). MDMA impairs response to water intake in healthy volunteers. Advances in pharmacological sciences
8. JR;, Grunau BE;Wiens MO;Brubacher. “Dantrolene in the Treatment of MDMA-Related Hyperpyrexia: A Systematic Review.” CJEM, U.S. National Library of Medicine, pubmed.ncbi.nlm.nih.gov/20880437/. Accessed 22 Oct. 2023.