By Chelsea Mikolowsky, PGY4
Patients at their end of life are encountered regularly in the ED and the opportunity to open up a discussion of patients’ wishes and goals of care, and to offer possible palliative care, are many. Although this continues to be an area many ED physicians receive little training in. This fact, combined with the various obstacles to calm, open, discussion with patients and families that ED physicians already face, and the difficulty that exists with prognosticating critical patients while still in the department, emergency physicians are often fighting an uphill battle in offering end-of life care that patients, families, and providers can be satisfied with. Covid-19 has also created an environment where resource allocation may create scenarios where patients are being denied interventions they desire. This post will seek to offer strategies to providing high quality care to the ED patient suffering from critical disease in the setting of COVID-19.
Approach to End-of Life in the ED
The palliative care literature offers many strategies and recommendations for delivering bad news of many kinds and opening a line of communication to address the patients’ needs in the face of critical illness. One of these is the SPIKES pneumonic.
- Setting- involves being prepared, goal oriented, and creating an environment for the conversation
- Perception- find out what they know- expectations understanding of condition, health literacy
- Invitation- get consent to give the news, find out what they want to know, ”Is it ok to speak directly/freely”
- Knowledge- lead directly with the point, speak to them on their level, provide information, ask what they think.
- Emotions/Empathy- identify emotions and address/ acknowledge them, validate responses
- Summarize Strategize- make a plan together and reaffirm GOC and commitment to care
Palliative care will always be a part of emergency medicine and it is important to develop a strategy to address patients concerns with regard to end-of -life care in all settings. The above can be difficult to implement in the ED. Ottawa EM blog offers a how-to guide to goals of care discussion in the ED which offers the following algorithm:
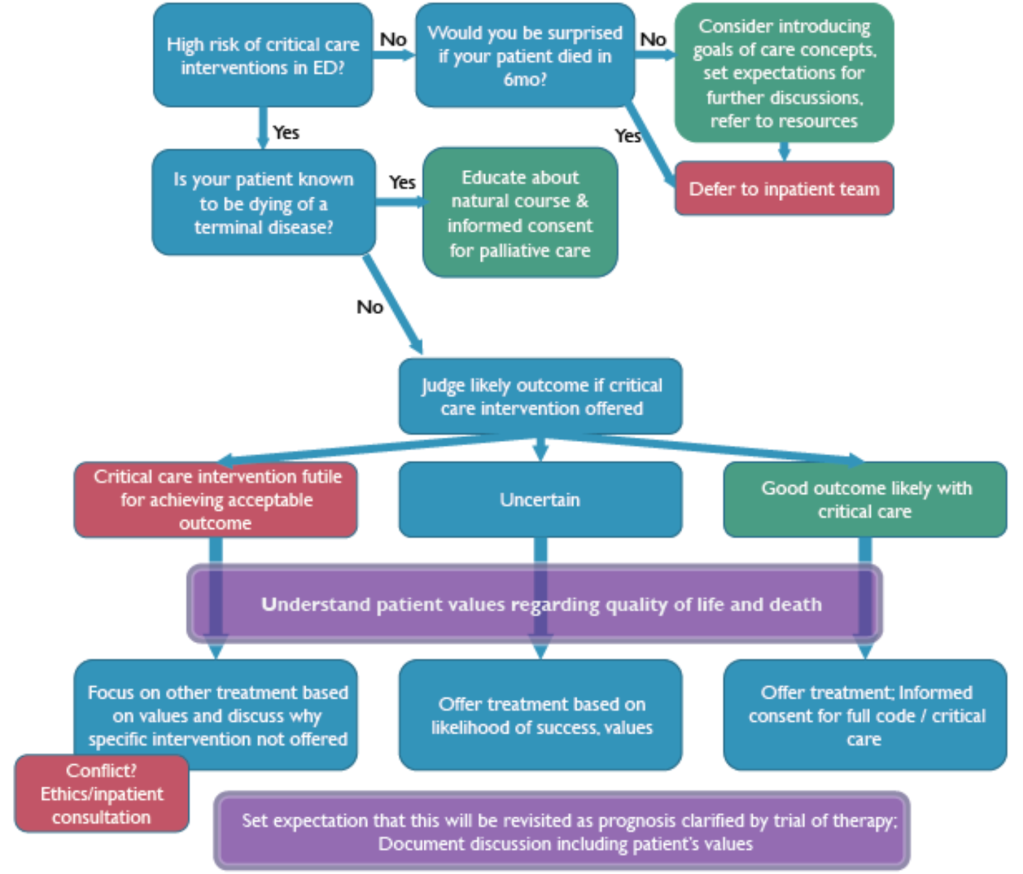
It goes on to break this algorithm down step by step to facilitate better ED management of GOC. Whichever strategy you chose, it is important to be comfortable addressing palliative care needs as an ED physician.
Special Considerations in COVID-19
Literature Review
Pandemic palliative care: beyond ventilators and saving lives. Arya et al. CMAJ April 14, 2020 192 (15)
This article from the Canadian Medical Association Journal offers strategies to address the increased need for palliative care in a pandemic and how emergency physicians may be prepared.
Authors explain that the COVID-19 pandemic will cause a greatly increased need for palliative care resources in addition to parallel the increased need for critical care. This will result from three factors: an increase in severely ill patients with comorbidities and who already have EOL care plans who will now be utilizing them in the setting of infection, those who receive critical interventions and do not improve, and if or when resources dwindle, those who are critically ill who will need to be denied critical care interventions. In this case the current force of palliative care providers will likely be insufficient and these duties will need to be taken on by ED physicians, ICU physicians, long term care workers, and family physicians as well as telehealth.
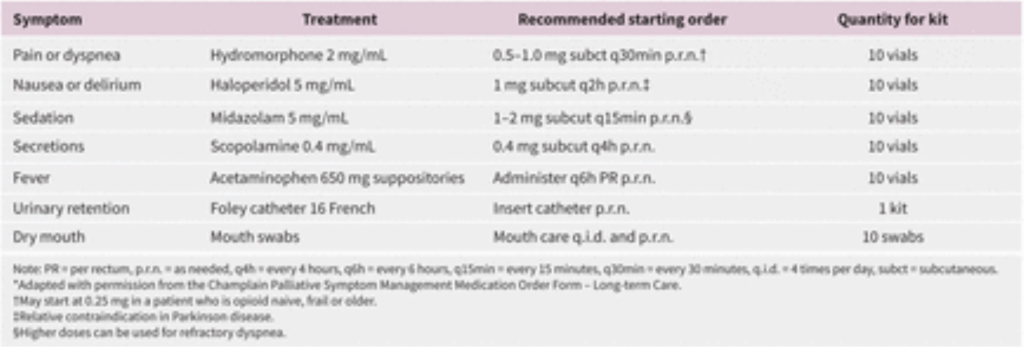
Authors recommend maximizing utilization of palliative services in the appropriate patient population only, as well as social work and pastoral support services, and that these other provider groups address palliative and EOL care needs themselves. They also recommend stockpiling palliative medications such as morphine and making “kits” to provide palliative care in the acute setting. They discuss taking special care to ensure that marginalized groups are receiving equal access to palliative services, triaging those who would benefit, and addressing family concerns associated with separation due to the pandemic. Lastly, they discuss setting aside space for palliative care units in addition to extra critical care space. These recommendations mirror the response strategy put forth by the US Task force for Mass Casualty Critical Care “stuff, staff, space, and systems:.
This chart addresses who should get a palliative medicine consult:
Clinicians who are not palliative care specialists (hospitalists, family physicians, internists, ICU physicians, nurse practitioners, nurses and paramedics) support the following:
- Identification and management of pain, dyspnea, agitated delirium and respiratory congestion
- Management of caregiver grief
- Discussions about prognosis, goals of treatment, suffering and resuscitation status
Palliative care specialist clinicians support the following:
- Patients with complex or refractory symptoms
- Patients who are denied access to critical care owing to a triage protocol, despite wanting aggressive care
- Management of complex depression, anxiety, grief and existential distress
- Requirement for palliative sedation therapy
- Pre-existing opioid use disorder
- Patients with young children
- Patients belonging to marginalized populations, including the homeless, incarcerated persons and Indigenous Peoples, who are at risk of being underserved by the health care system
Helpful to ED physicians, the article also reviews palliative management of symptoms commonly encountered in COVID-19 to help providers address patient comfort appropriately regardless of whether it not they receive critical interventions. Below is a chart addressing dosing of palliative medications and symptoms.
End-of-life care in the emergency department for the patient imminently dying of a highly transmissible acute respiratory infection (such as COVID-19) Hendin et. Al CJEM. 2020 Mar 26 : 1–4.
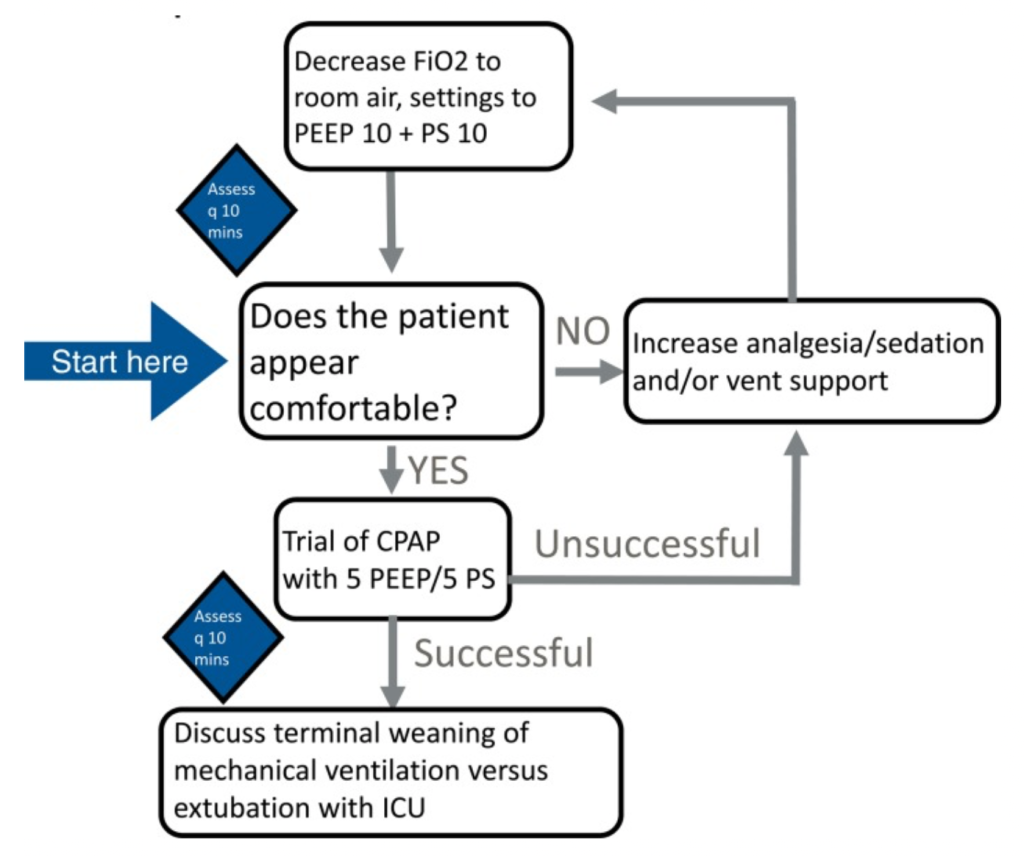
This article from the Canadian Journal of Emergency Medicine also recognizes the growing responsibility to provide palliative care to a rapidly increasing base of patients near end-of-life in the current pandemic. Authors make recommendations to adjustments that must be made to standard palliative practices to adapt to the current environment. These include changes to nursing ratios to compensate for increased care needed for dying patients as well as time required to take appropriate viral precautions, as well as increasing debriefings to maintain communication and concern for the well-being of emergency staff. This article also encourages comfort in emergency physicians with administering palliative medications as well as the management of terminal ventilator weaning. A guide to terminal vent management is provided below. Currently, as it is an aerosolizing procedure, it is recommended to withhold terminal extubation in the ED if possible, and instead to wean vent support and maintain comfort. Lastly, they continue to recommend involving chaplaincy and social work often and utilize video conferencing with family as often as possible when visitation is limited.
The goals of palliative care should not change during a pandemic, but the execution may begin to look slightly different. Emergency physicians will likely find themselves more responsible for providing this care then previously, and they should take steps to be prepared to handle this responsibility adequately.
Terminal Weaning of Ventilatory Support
More Resources For Emergency Physicians
Covid Ready Communication Playbook- collection of commonly discussed topics between providers and patients in the COVID-19 pandemic, such as access to testing, end of life considerations, and resource allocation from Vital Talks, a non-profit group out of Seattle which offers education for physicians regarding communication skills and crowdsourced a compilation of appropriate answers to many COVID questions. https://www.vitaltalk.org/guides/covid-19-communication-skills/
A 5 minute video of involving a GOC discussion with a family surrogate for a COVID-19 patient- https://vimeo.com/401465080
Ottawa EM Blog- How-To Guide for EOL Discussions in the ED- https://emottawablog.com/2019/04/a-how-to-guide-to-goals-of-care-discussions-in-the-emergency-department/
References
Arya et al, Pandemic palliative care: beyond ventilators and saving lives CMAJ April 14, 2020 192 (15) E400-E404; DOI: https://doi.org/10.1503/cmaj.200465
Hendin et. al, End-of-life care in the emergency department for the patient imminently dying of a highly transmissible acute respiratory infection (such as COVID-19) CJEM. 2020 Mar 26 : 1–4.
Sethuarman, Shankur. A HOW-TO GUIDE TO GOALS OF CARE DISCUSSIONS IN THE EMERGENCY DEPARTMENT. Ottawa EM Blog. https://emottawablog.com/2019/04/a-how-to-guide-to-goals-of-care-discussions-in-the-emergency-department/
Hayes, Kaitlyn, Palliative Care and Advance Care Planning Resources for ED Physicians during the COVID-19 pandemic. CanadienEM. https://canadiem.org/palliative-care-resources-for-ed-physicians-during-the-covid-19-pandemic/
Kaplan M. SPIKES: a framework for breaking bad news to patients with cancer. Clin J Oncol Nurs. 2010 Aug;14(4):514-6. doi: 10.1188/10.CJON.514-516.